Extending Our Understanding of the Social Determinants of Physical Activity and Sedentary Behaviors in Families: A Systems Mapping Approach
November 14, 2024
Comparing Multiple Approaches to Estimate Physical Activity, Sedentary Behavior, and Sleep in Pregnancy
November 28, 2024Congratulations to Dr. Andrew Agbaje and colleagues for their new study entitled, “Lean Mass Longitudinally Confounds Sedentary Time and Physical Activity With Blood Pressure Progression in 2513 Children” just published in J Cachexia Sarcopenia Muscle. A big thank you also goes to Dr. Andrew Agbaje who provided this blog post. This press release was originally published by the University of Eastern Finland which can be found here. Full link to the article can be found here.
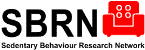
Time spent sedentary beyond six hours per day during growth from childhood through young adulthood may cause an excess increase of 4 mmHg in systolic blood pressure, a new study shows. Continuously engaging in light physical activity (LPA) significantly mitigated the rise in blood pressure. The study was conducted in collaboration between the Universities of Bristol and Exeter in the UK, and the University of Eastern Finland, and the results were published in the prestigious Journal of Cachexia, Sarcopenia and Muscle.
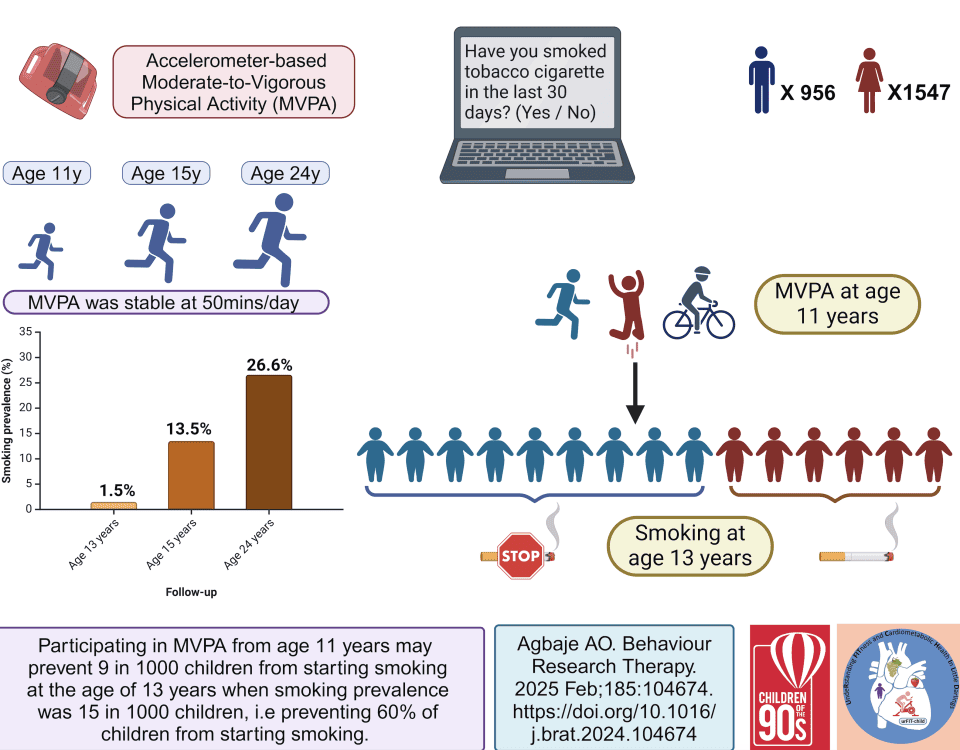
In the present study, 2,513 children drawn from the University of Bristol’s Children of the 90s cohort were followed up from age 11 until 24 years. At baseline, the children spent six hours per day sedentary, six hours per day engaging in LPA, and approximately 55 minutes per day in moderate-to-vigorous physical activity (MVPA). At follow-up in young adulthood, nine hours per day were spent sedentary, three hours per day in LPA, and approximately 50 minutes per day in MVPA.
The average blood pressure in childhood was 106/56 mmHg which increased to 117/67 mmHg in young adulthood, partly due to normal physiological development. Persistent increase in sedentary time from age 11 through 24 years was associated with an average of 4 mmHg excess increase in systolic blood pressure. Participating in LPA from childhood lowered the final level by 3 mmHg, but engaging in MVPA had no blood pressure-lowering effect.
“Furthermore, when 10 minutes out of every hour spent sedentary was replaced with an equal amount of LPA from childhood through young adulthood in a simulation model, systolic blood pressure decreased by 3 mmHg and diastolic blood pressure by 2 mmHg. This is significant, as it has been reported in adults that a systolic blood pressure reduction of 5 mmHg decreases the risk of heart attack and stroke by ten percent,” says Andrew Agbaje, an award-winning physician and associate professor (docent) of Clinical Epidemiology and Child Health at the University of Eastern Finland.
The current study is the largest and the longest follow-up of accelerometer-measured movement behaviour and blood pressure progression in youth in the world. Measurements of blood pressure, sedentary time, LPA and, MVPA were taken at ages 11, 15, and 24 years. The children’s fasting blood samples were also repeatedly measured for low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, glucose, insulin, and high-sensitivity C-reactive protein. Heart rate, socio-economic status, family history of cardiovascular disease, smoking status as well as dual-energy X-ray absorptiometry measured fat mass and lean mass were accounted for in the analyses.
“We have earlier shown that elevated blood pressure and hypertension in adolescence increase the risk of premature cardiac damage in young adulthood. The identification of childhood sedentariness as a potential cause of elevated blood pressure and hypertension with LPA as an effective antidote is of clinical and public health significance. Several MVPA-based randomised controlled trials in the young population have been unsuccessful in lowering blood pressure. We noted an MVPA-induced increase in muscle mass enhanced a physiologic increase in blood pressure explaining why earlier MVPA-based randomised clinical trials were unsuccessful,” says Agbaje.
“The World Health Organization estimates that 500 million new cases of physical inactivity-related non-communicable diseases would occur by 2030 and half would result from hypertension. At least three hours of LPA per day is critical to preventing and reversing elevated blood pressure and hypertension. Examples of LPA are long walks, house chores, swimming, and bicycling. We all, parents, paediatricians and policymakers included, should encourage children and adolescents to participate in LPA to keep their blood pressure in a healthy range,” Agbaje concludes.
Agbaje’s research group (urFIT-child) is supported by research grants from Jenny and Antti Wihuri Foundation, the Finnish Cultural Foundation Central Fund, the Finnish Cultural Foundation North Savo Regional Fund, the Orion Research Foundation, the Aarne Koskelo Foundation, the Antti and Tyyne Soininen Foundation, the Paulo Foundation, the Yrjö Jahnsson Foundation, the Paavo Nurmi Foundation, the Finnish Foundation for Cardiovascular Research, Ida Montin Foundation, Eino Räsänen Fund, Matti and Vappu Maukonen Fund, Foundation for Pediatric Research, Alfred Kordelin Foundation and Novo Nordisk Foundation.
In 2513 children followed up from age 11 to 24 years, increased sedentary time from childhood through young adulthood significantly increased systolic blood pressure. However, a simulation replacing 10 minutes every hour of sedentary time in childhood, adolescence, and young adulthood with 10 minutes of light physical activity resulted in a cumulative reduction of systolic blood pressure by -3 mmHg. Image: Andrew Agbaje.
For further information, please contact:
Andrew Agbaje, MD, MPH, PhD, FESC, FAHA, Cert. Clinical Research (Harvard), Professor (associate) of Clinical Epidemiology and Child Health, Principal Investigator (urFIT-child). Institute of Public Health and Clinical Nutrition, School of Medicine, University of Eastern Finland, Kuopio, Finland. andrew.agbaje(a)uef.fi, +358 46 896 5633
Honorary Research Fellow – Children’s Health and Exercise Research Centre, Public Health and Sports Sciences Department, Faculty of Health and Life Sciences, University of Exeter, Exeter, UK. a.agbaje@exeter.ac.uk
https://uefconnect.uef.fi/en/person/andrew.agbaje/
Webpage:
Link to the articles:
Agbaje AO. Lean Mass Longitudinally Confounds Sedentary Time and Physical Activity With Blood Pressure Progression in 2513 Children. J Cachexia Sarcopenia Muscle. 2024 Nov 13. doi: 10.1002/jcsm.13639. Epub ahead of print. PMID: 39535381
Other relevant articles:
Agbaje AO, Perng W, and Tuomainen TP. Effects of accelerometer-based sedentary time and physical activity on DEXA-measured fat mass in 6059 children. Nature Communications 14, 8232 (2023), December 12. https://doi.org/10.1038/s41467-023-43316-w
Agbaje AO. Associations of Sedentary Time and Physical Activity from Childhood with Lipids: A 13-Year Mediation and Temporal Study. The Journal of Clinical Endocrinology & Metabolism. 2024 Jun 17;109(7):e1494-e1505. https://doi.org/10.1210/clinem/dgad688
Videos and podcasts on childhood sedentariness
University of Eastern Finland video on the danger of sedentariness
University of Eastern Finland podcast on light physical activity
Endocrine Society podcast on the danger of sedentariness
BBC Radio Devon interview on the danger of sedentariness
DocCheck Video on the benefit of light physical activity
CNN news on the danger of sedentariness
About Children of the 90s
Based at the University of Bristol, Children of the 90s, also known as the Avon Longitudinal Study of Parents and Children (ALSPAC), is a long-term health research project that enrolled more than 14,000 pregnant women in 1991 and 1992. It has been following the health and development of the parents, their children and now their grandchildren in detail ever since. It receives core funding from the Medical Research Council, the Wellcome Trust and the University of Bristol.
About the University of Eastern Finland
The University of Eastern Finland, UEF, is the most multidisciplinary university in Finland. The university’s high standard of interdisciplinary research and education responds to global challenges, building a sustainable future. Research conducted at UEF is ranked among the best in the world in several fields. The university is home to 16,000 students and 3,200 staff.
For further information, please contact:
Andrew Agbaje, MD, MPH, PhD, FESC, FAHA, Cert. Clinical Research (Harvard), Professor (associate) of Clinical Epidemiology and Child Health, Principal Investigator (urFIT-child). Institute of Public Health and Clinical Nutrition, School of Medicine, University of Eastern Finland, Kuopio, Finland. andrew.agbaje(a)uef.fi, +358 46 896 5633
Honorary Research Fellow – Children’s Health and Exercise Research Centre, Public Health and Sports Sciences Department, Faculty of Health and Life Sciences, University of Exeter, Exeter, UK. a.agbaje@exeter.ac.uk
https://uefconnect.uef.fi/en/person/andrew.agbaje/